Life or death for a young child too often depends on whether he is born in a country where vaccines are available or not
– Nelson Mandela
Mycobacterium tuberculosis (TB) is a disease that has persisted throughout the years and continues to have a grip on public health worldwide (“Tuberculosis: Causes, Symptoms, Diagnosis & Treatment”). While it is a preventable, treatable infection, TB continues to be one of the deadliest infectious diseases worldwide, second only to COVID-19 (World Health Organization).
Each year, millions are affected despite the existence of a vaccine, the Bacillus Calmette-Guérin (BCG) vaccine, which has already proven effective in reducing the severity of TB infections. But why does TB remain so widespread despite it being treatable? The answer lies in a complex mix of limited healthcare access, poverty, and a lack of awareness, factors that make it difficult for many to seek early diagnosis and treatment. To bridge this gap, establishing outreach centers in underserved areas could be the key to turning the tide against TB, ensuring that vaccinations, healthcare, and education reach those who need it most.
What is Mycobacterium tuberculosis?
Mycobacterium tuberculosis is a pathogen/parasite. A pathogen is any agent capable of causing an infection; this can include: viruses, bacteria, fungi, and even infectious proteins called prions. Different pathogens can utilize mechanisms to enter a host, evade the host’s immune system, and consequently, wreak havoc on the host’s internal environment. (Alberts et al.). M. tuberculosis specifically spreads through prolonged contact with an individual with active TB. The release of respiratory droplets, tiny liquid particles expelled from the respiratory tract when a person breathes, talks, coughs, sneezes, or laughs, by these infected individuals results in infection (“Tuberculosis: Causes, Symptoms, Diagnosis & Treatment”).
The initial site of infection by TB is the alveoli. Initially, our immune systems are sufficient to fight the bacterium and prevent its growth, forcing it into a latent state. The danger, however, lies in if the individual’s immune system becomes weakened enough and can no longer prevent TB growth, at this stage, TB becomes active. Symptoms of active TB include persisting coughing, coughing of blood/mucous, weight loss, fever, chills, and fatigue/weakness (“Tuberculosis: Causes, Symptoms, Diagnosis & Treatment”). These symptoms not only mark a serious health decline for the infected individual but also increase the risk of transmission to others, especially in crowded or poorly ventilated environments via coughing. Without timely diagnosis and treatment, active TB can spread rapidly through communities, underscoring the critical need for awareness, early detection, and access to effective healthcare interventions.
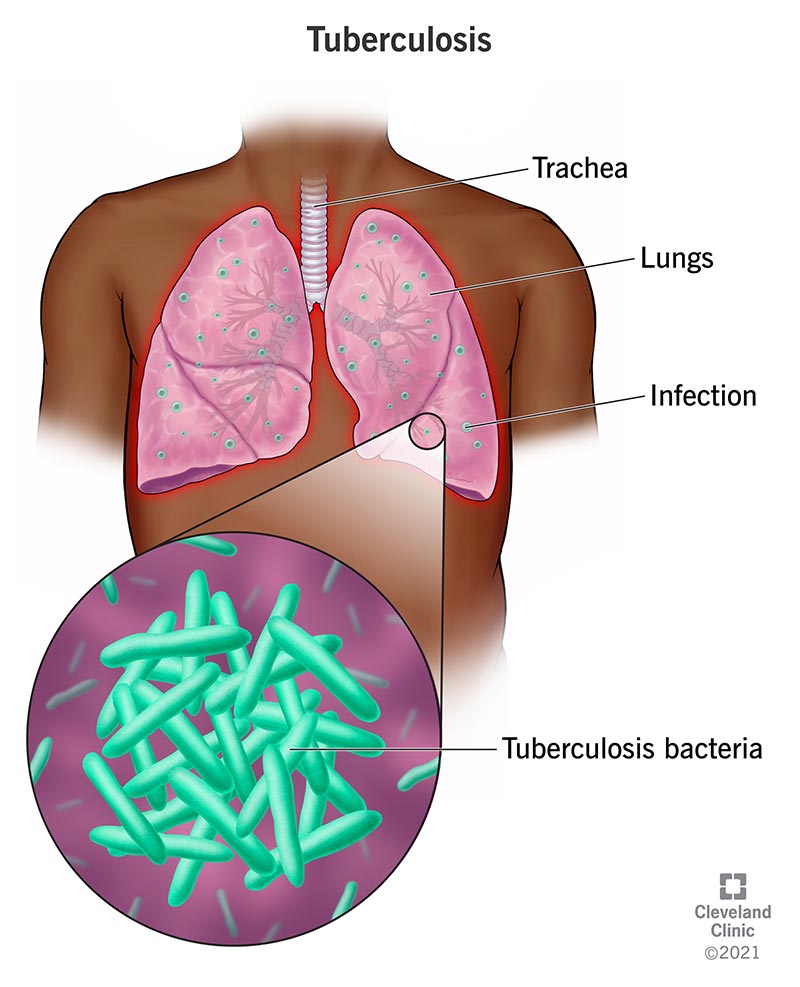
M.tuberculosis, Image obtained from Cleveland Clinic
M.tuberculosis as a health concern
Tuberculosis (TB) remains a critical global health threat and ranked as the 10th leading cause of death worldwide in 2021, and the second leading infectious killer after COVID-19, surpassing even HIV and AIDS (World Health Organization). The burden of TB is particularly high in low- and middle-income countries like the Democratic Republic of Congo, India, Iran, Mexico, and Nigeria, where limited healthcare access exacerbates the disease’s impact (World Health Organization). But TB is not limited by borders; in 2021 alone, there were 1,829 reported cases of active TB in Canada (Government of Canada) and 8,331 reported cases in the United States (CDC), highlighting its persistence even in high-income countries.
Consequently, only about two in five people with drug-resistant TB were able to access the necessary treatment in 2022 (World Health Organization), emphasizing the urgent need for strengthened global efforts in prevention, early diagnosis, and access to effective treatment to curb this escalating threat. This becomes more imperative as TB becomes increasingly resistant to standard treatments, with multidrug-resistant strains now posing a major public health crisis and health security threat. In which in 2022, approximately 410,000 individuals developed multidrug-resistant or rifampicin-resistant tuberculosis. Although the treatment rate for this form of TB has increased to 60%, the World Health Organization still regards this figure as low, emphasizing the importance of vaccination (World Health Organization).
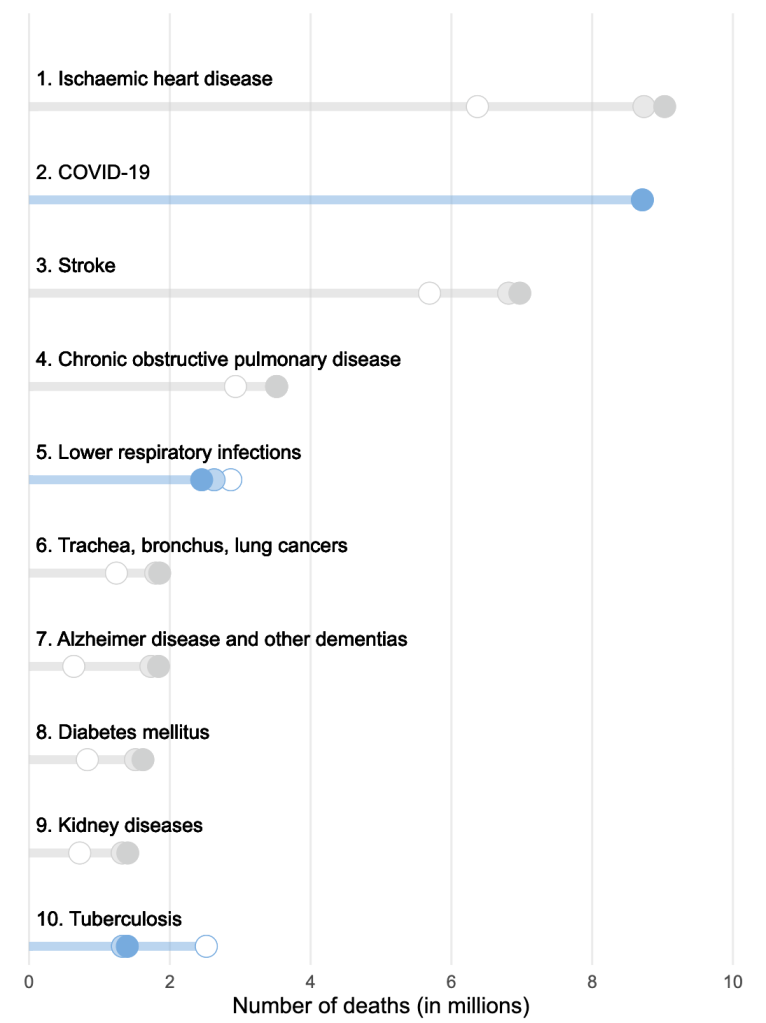
Leading causes of death in 2021, image obtained from WHO
Barriers to treatment-seeking
Barriers to seeking treatment for tuberculosis (TB) are significant, particularly in lower-middle-income countries, where individuals often face considerable healthcare access challenges. There are often disparities in healthcare expertise in disenfranchised communities (Olufadewa et al.), including those in low-middle-income countries (LMICs), and high-income countries (HICs). For instance, of the 1,829 cases of TB in Canada, 232 out of 321 Canadian-born cases were in Indigenous communities (Government of Canada), suggesting a severe lack of culturally appropriate healthcare services and targeted support for marginalized populations.
Funding and sustainability in healthcare remain a worldwide issue. Many healthcare programs in LMICs rely on short-term, irregular funding, often from foreign donors. Establishing local outreach centers within these LMICs could help create more stable, community-centered care networks, fostering long-term healthcare access and reducing reliance on external funding sources (Olufadewa et al.).
In both LMICs and HICs as well, the costs of treatment for TB may deter many, especially disenfranchised individuals who may not have access to insurance, a factor which may deter them from seeking treatment. Additionally, education plays a crucial role in this issue, as many individuals are unaware of TB symptoms and the severity of the disease if left untreated, which can lead to dangerous delays in seeking medical attention. This combination of factors hampers individual health outcomes and perpetuates the cycle of transmission within communities.
Importance of Vaccinations and Outreach Centres
Establishing outreach centers is vital for improving access to tuberculosis (TB) treatment and vaccination, particularly in underserved communities (Olufadewa et al.). The TB vaccine, Bacille Calmette-Guérin (BCG), has an estimated 51% efficacy in preventing any TB disease and up to 78% in protecting newborns from miliary (disseminated) or meningeal TB (Government of Canada). Therefore, the fact that the efficacy rate of the BCG vaccine is so high, yet TB remains a global issue suggests a lack of distribution/education. These outreach centers, however, would enhance accessibility by bringing healthcare services directly to individuals, effectively ensuring that all communities, especially those who have been disenfranchised, receive adequate levels of care tailored towards their specific communities. Additionally, outreach centers/organizations play a crucial role in raising awareness about TB symptoms and the importance of early treatment, empowering communities with the knowledge needed to combat the disease.
The World Health Organization (WHO) over the years has established guidelines for TB utilizing what they call the “GRADE” method (Grading of Recommendations Assessment, Development, and Evaluation), these guidelines are grounded in evidence on various aspects of TB prevention, screening, diagnosis, and treatment. By establishing these guidelines and offering comprehensive courses that address various aspects of tuberculosis, WHO has actively sought to ensure that healthcare professionals, especially those on the front lines of healthcare worldwide, have access to accurate, detailed, and practical information. This approach aims to educate communities and help laypeople understand when it is necessary to seek treatment and the different treatment options available to them.
Tuberculosis remains a global health challenge, affecting millions despite being a preventable and treatable disease. The persistence of TB highlights the urgent need for improved healthcare accessibility, especially in LMICs, where factors like limited resources, and lack of awareness hinder effective diagnosis and treatment. With the guidance of global health organizations like WHO, which continues to provide evidence-based frameworks and training, and the establishment of local outreach treatment centers, we can work to cultivate stronger community responses to TB. Addressing the barriers that have allowed TB to thrive demands ongoing commitment and collaboration, but with sustained action, we can make significant strides toward a future where TB no longer poses a threat to public health worldwide.
Works Cited
Alberts, Bruce, et al. “Introduction to Pathogens.” Nih.gov, Garland Science, 2024, http://www.ncbi.nlm.nih.gov/books/NBK26917/.
CDC. “Reported TB in the U.S., 2021- National Data.” Centers for Disease Control and Prevention, 15 Nov. 2023, http://www.cdc.gov/tb/statistics/reports/2022/national_data.htm#:~:text=Reported%20Tuberculosis%20in%20the%20United%20States%2C%202022&text=In%202022%2C%20the%20United%20States,incidence%20rate%20compared%20with%202021.
“Item.” Who.int, 2024, http://www.who.int/news-room/questions-and-answers/item/tuberculosis-multidrug-resistant-tuberculosis-(mdr-tb)#:~:text=Multidrug%2Dresistant%20TB%20(MDR%2DTB)%20is%20a%20form,resistant%20to%20rifampicin%20and%20isoniazid.
Olufadewa, Isaac, et al. “Global Health in Low-Income and Middle-Income Countries: A Framework for Action.” The Lancet Global Health, vol. 9, no. 7, 15 June 2021, pp. e899–e900, http://www.thelancet.com/journals/langlo/article/PIIS2214-109X(21)00143-1/fulltext, https://doi.org/10.1016/s2214-109x(21)00143-1.
Public. “Bacille Calmette-Guérin (BCG) Vaccine: Canadian Immunization Guide – Canada.ca.” Canada.ca, 2014, http://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-4-active-vaccines/page-2-bacille-calmette-guerin-vaccine.html.
“Tuberculosis: Causes, Symptoms, Diagnosis & Treatment.” Cleveland Clinic, 29 Dec. 2016, my.clevelandclinic.org/health/diseases/11301-tuberculosis.
“Tuberculosis (TB): Monitoring – Canada.ca.” Canada.ca, 2021, http://www.canada.ca/en/public-health/services/diseases/tuberculosis/surveillance.html.
“Tuberculosis in Canada: Infographic (2021) – Canada.ca.” Canada.ca, 2021, http://www.canada.ca/en/public-health/services/publications/diseases-conditions/tuberculosis-canada-2021-infographic.html.
“Tuberculosis: Causes, Symptoms, Diagnosis & Treatment.” Cleveland Clinic, 29 Dec. 2016, my.clevelandclinic.org/health/diseases/11301-tuberculosis.
“Understanding and Using WHO Guidelines on Tuberculosis.” OpenWHO, 2016, openwho.org/courses/who-gtb-guidelines. Accessed 29 Oct. 2024.World. “The Top 10 Causes of Death.” Who.int, World Health Organization: WHO, 7 Aug. 2024, http://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
Written by: Salamat Ibrahim
